CRP is a key part of the immune and inflammatory response
This crucial biomarker, known as C-reactive protein (CRP), offers valuable insights into the body's inflammatory response.
August 10, 2023
6 min read
Key takeaways
- CRP is a protein that is part of the immune response and increases when infection occurs.
- Acting as a sign of inflammation, CRP rises in both acute and chronic conditions.
- CRP is important because it protects against pathogens and can be used to determine disease risk and prognosis.
- Poor mitochondrial functioning has been linked to elevated levels of CRP, yet additional research is needed to understand the relationship between mitochondrial health, inflammation, and CRP levels.
- Further study in this area will allow for the development of new therapies to address inflammatory conditions.

What is CRP?
C-reactive protein (CRP) was identified in 1930 and is produced primarily in the liver but also in other cells, including muscle and fat.[1] CRP is considered an "acute phase protein," as it provides an early indication of infection and inflammation. As a Pattern Recognition Receptor (PRR) protein, it can recognize molecules found in pathogens and, as such, can be used as a way to screen for inflammation and act as a marker for disease.[2]
Given that CRP increases rapidly after tissue injury or infection, it is considered part of the immune response and the body’s defense system. CRP actively interacts with and elicits a reaction from other cells in the presence of pathogens, contributing to the first line of host defense. It has been shown to play a protective role in bacterial and other types of infection.[3]
CRP has garnered attention lately as a tool for evaluating the risk of developing diseases, but measuring it involves several important considerations. Numerous factors can influence CRP levels, such as cigarette smoking, obesity, insulin resistance, diabetes, hypertension, poor physical conditioning, hypertriglyceridemia, and even depression. Furthermore, some people may have a genetic predisposition that leads to higher baseline CRP levels.[4] Therefore, when assessing CRP levels and drawing conclusions about one's health status, it becomes crucial to consider these factors.
What is the role of CRP in inflammation?
CRP has been found to increase up to 1,000-fold at sites of infection or inflammation, and there is evidence that it plays an essential role in the inflammatory process.[5] Elevated levels of CRP have been found in inflammatory conditions such as rheumatoid arthritis and cardiovascular disease.[6] Some bacterial infections have also been shown to increase levels significantly.[7]
CRP is considered a marker of inflammation, playing a vital role in orchestrating the inflammatory response.[8] Acting as a surveillance molecule elicits an early adaptive immune system defense cascade. CRP binds to damaged cell membranes and pathogenic organisms and encourages the release of pro-inflammatory cytokines - substances that affect other cells.[9]
Why is CRP important?
CRP protects against infection, with several studies demonstrating its protective effect against different pathogens, and its role in phagocytosis is a key part of the protection it provides.
Phagocytosis is the cellular process that allows for the elimination of cellular particles, such as foreign substances.[10] CRP effectively promotes an increase in phagocytosis, acting as a constituent in the first-line defense against pathogens.[11]
CRP also plays a role in the vital processes of apoptosis, the programmed cell death essential for immune function. Research has demonstrated that CRP stimulates the production of cytokines that promote apoptosis. This process is important as a defense mechanism and to maintain the homeostasis of cells.[12]
As CRP levels are elevated in certain disease states, it can be valuable in determining disease risk and prognosis. CRP levels have been linked to prognosis in patients with atherosclerotic disease, congestive heart failure, atrial fibrillation, myocarditis, aortic valve disease, and heart transplantation, and elevated levels may be used to indicate risk for conditions such as coronary heart disease.[13]
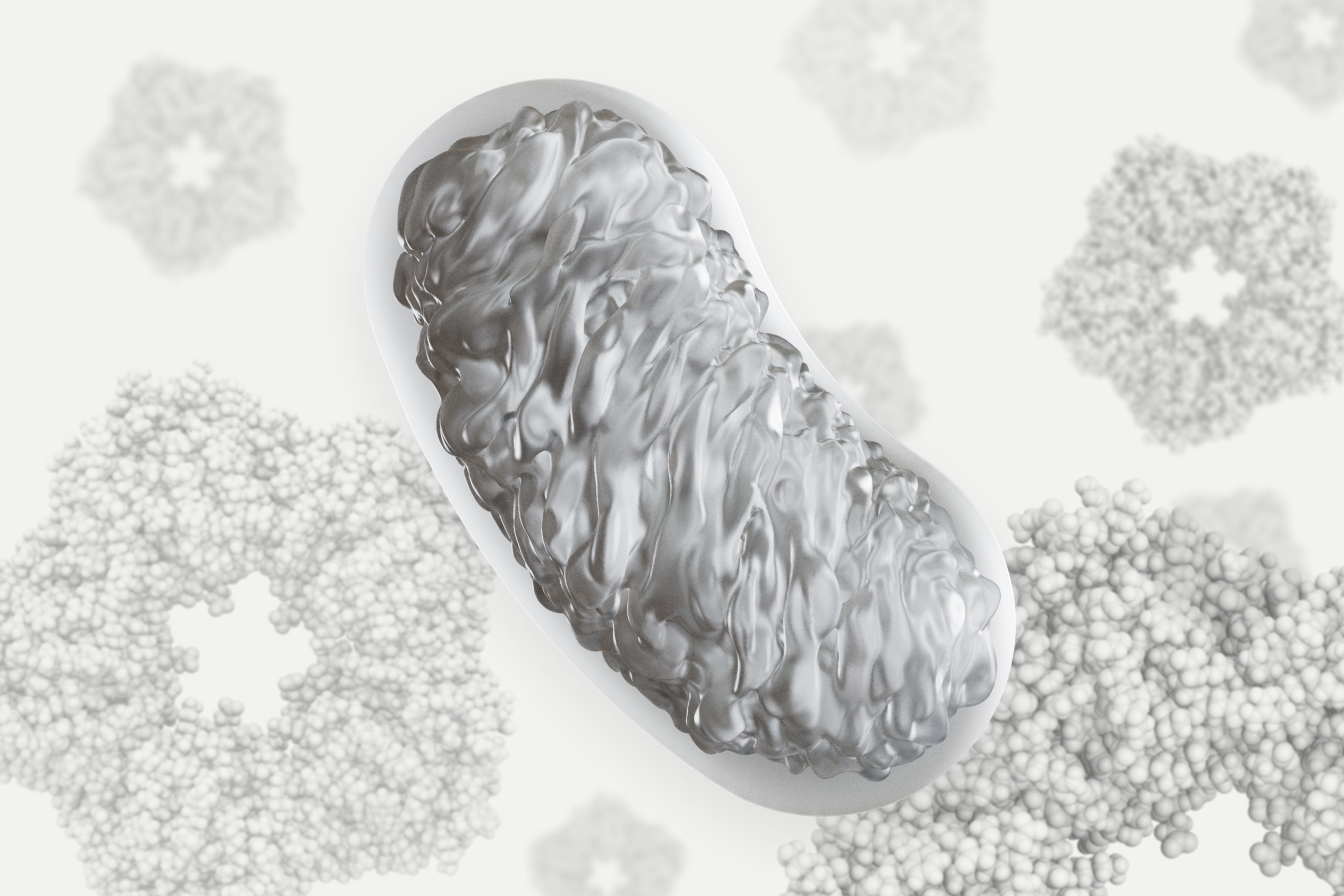
Artist illustration of a bad mitochondrion surrounded by CRPs
How does CRP relate to mitochondrial health?
As the site of energy production, mitochondria are considered the “powerhouse” of the cell.
Recent research found that poor mitochondrial functioning is associated with elevated levels of CRP.[14] It is unclear whether inflammation causes mitochondrial dysfunction or whether dysfunctional mitochondria directly cause inflammation; however, this study demonstrated that individuals with mitochondrial dysfunction showed signs of inflammation.
As some researchers believe that chronic, low-grade inflammation may have long-term effects on health,[15] and the mitochondria play a role in the inflammatory response. It is important to conduct further studies to better understand this complex relationship, as mitochondrial dysfunction has implications for how we age, impacting immune response and organ functioning. A better understanding of these relationships will allow for the development of new therapies for infections and chronic inflammatory diseases.[16]
References
- ↑
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754. PMID: 29706967; PMCID: PMC5908901.
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999 Nov-Dec;17(6):1019-25. doi: 10.1016/s0736-4679(99)00135-3. PMID: 10595891.
- ↑
Clyne B, Olshaker JS. The C-reactive protein. J Emerg Med. 1999 Nov-Dec;17(6):1019-25. doi: 10.1016/s0736-4679(99)00135-3. PMID: 10595891.
- ↑
Black S, Kushner I, Samols D. C-reactive Protein. J Biol Chem. 2004 Nov 19;279(47):48487-90. doi: 10.1074/jbc.R400025200. Epub 2004 Aug 26. PMID: 15337754.
- ↑
Kushner I, Rzewnicki D, Samols D. What does minor elevation of C-reactive protein signify? Am J Med. 2006 Feb;119(2):166.e17-28. doi: 10.1016/j.amjmed.2005.06.057. PMID: 16443421.
- ↑
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754. PMID: 29706967; PMCID: PMC5908901.
- ↑
Du Clos TW, Mold C. C-reactive protein: an activator of innate immunity and a modulator of adaptive immunity. Immunol Res. 2004;30(3):261-77. doi: 10.1385/IR:30:3:261. PMID: 15531769.
- ↑
Thompson D, Pepys MB, Wood SP. The physiological structure of human C-reactive protein and its complex with phosphocholine. Structure. 1999 Feb 15;7(2):169-77. doi: 10.1016/S0969-2126(99)80023-9. PMID: 10368284.
- ↑
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754. PMID: 29706967; PMCID: PMC5908901.
- ↑
Du Clos TW. Function of C-reactive protein. Ann Med. 2000 May;32(4):274-8. doi: 10.3109/07853890009011772. PMID: 10852144.
Kaplan MH, Volanakis JE. Interaction of C-reactive protein complexes with the complement system. I. Consumption of human complement associated with the reaction of C-reactive protein with pneumococcal C-polysaccharide and with the choline phosphatides, lecithin and sphingomyelin. J Immunol. 1974 Jun;112(6):2135-47. PMID: 4151108.
- ↑
Uribe-Querol E, Rosales C. Phagocytosis: our current understanding of a universal biological process. Frontiers in immunology. 2020 Jun 2;11:1066.
- ↑
Black S, Kushner I, Samols D. C-reactive Protein. J Biol Chem. 2004 Nov 19;279(47):48487-90. doi: 10.1074/jbc.R400025200. Epub 2004 Aug 26. PMID: 15337754.
- ↑
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018 Apr 13;9:754. doi: 10.3389/fimmu.2018.00754. PMID: 29706967; PMCID: PMC5908901.10.1161/01.ATV.0000168573.10844.ae. Epub 2005 Apr 28. PMID: 15860734.
- ↑
Osman R, L'Allier PL, Elgharib N, Tardif JC. Critical appraisal of C-reactive protein throughout the spectrum of cardiovascular disease. Vasc Health Risk Manag. 2006;2(3):221-37. doi: 10.2147/vhrm.2006.2.3.221. PMID: 17326329; PMCID: PMC1993979.
- ↑
Zampino M, Brennan NA, Kuo PL, Spencer RG, Fishbein KW, Simonsick EM, Ferrucci L. Poor mitochondrial health and systemic inflammation? Test of a classic hypothesis in the Baltimore Longitudinal Study of Aging. Geroscience. 2020 Aug;42(4):1175-1182. doi: 10.1007/s11357-020-00208-x. Epub 2020 Jun 22. PMID: 32572752; PMCID: PMC7394984.
- ↑
Del Giudice M, Gangestad SW. Rethinking IL-6 and CRP: Why they are more than inflammatory biomarkers, and why it matters. Brain Behav Immun. 2018 May;70:61-75. doi: 10.1016/j.bbi.2018.02.013. Epub 2018 Mar 1. PMID: 29499302.
- ↑
Andrieux P, Chevillard C, Cunha-Neto E, Nunes JPS. Mitochondria as a Cellular Hub in Infection and Inflammation. Int J Mol Sci. 2021 Oct 20;22(21):11338. doi: 10.3390/ijms222111338. PMID: 34768767; PMCID: PMC8583510.
Authors
Jinan Banna
Author